Waking up with crusty eyelashes or feeling like there is sand in your eyes can be more than just tiredness. Blepharitis is a chronic inflammation of the eyelids. It is common, and prevalence estimates vary by study and population.
Explore the full overview in the Blepharitis symptoms and diagnosis hub.
Symptom Assessment Tool
Important Medical Disclaimer:
This tool is for educational and informational purposes only. It is not a diagnostic device and does not provide medical advice. Using this tool does not create a physician-patient relationship.
This short assessment helps categorize your symptoms to direct you to the most relevant educational articles on our site.
"Blepharitis and dry eye often overlap, and symptoms can look similar. A slit-lamp exam helps clarify what's driving symptoms."
Key Symptoms to Watch For
Blepharitis symptoms are typically worse in the morning. The condition typically affects both eyes. If you are experiencing persistent discomfort, check for these common indicators:

- Red, swollen eyelids: The margins of your eyelids may appear inflamed or greasy.
- Crusts or flakes: Look for dandruff-like scales at the base of your eyelashes (collarettes).
- Gritty sensation: A feeling that something is in your eye (foreign body sensation).
- Photophobia: Mild sensitivity to bright lights.
- Frequent styes: Recurring painful red lumps near the eyelid edge.
Blepharitis stages (a practical way to think about flares)
There isn't a universally used staging system in routine practice. Some people find it helpful to think in terms of milder symptoms vs flares vs longer-term gland changes.
- Early irritation: Mild itching, dryness, and subtle lid margin redness that comes and goes.
- Active flare: Noticeable crusting, swelling, and burning, often worse on waking.
- Chronic changes: Ongoing gland blockage, thicker oils, and recurrent styes or chalazia.
Self-Check Tip
Look closely at your eyelash line in a mirror with good lighting. If you see tiny, tubular crusts surrounding the base of the lashes, collarettes can be a strong clue for Demodex blepharitis, but confirmation typically involves a clinician exam (and sometimes lash sampling).
Anterior vs. Posterior: What's the Difference?
Doctors classify blepharitis into two main types based on which part of the eyelid is affected. It is possible (and common) to have both simultaneously.
1. Anterior Blepharitis
This affects the outside front of the eyelid, where the eyelashes attach.
- Staphylococcal: Caused by an overgrowth of bacteria (Staphylococcus) that naturally live on the skin. It often causes hard crusts and can lead to lash loss.
- Seborrheic: Associated with dandruff of the scalp and eyebrows. The scales are typically greasy and soft.
2. Posterior Blepharitis (MGD)
This affects the inner eyelid margin that touches the eyeball. It is primarily caused by Meibomian Gland Dysfunction (MGD).
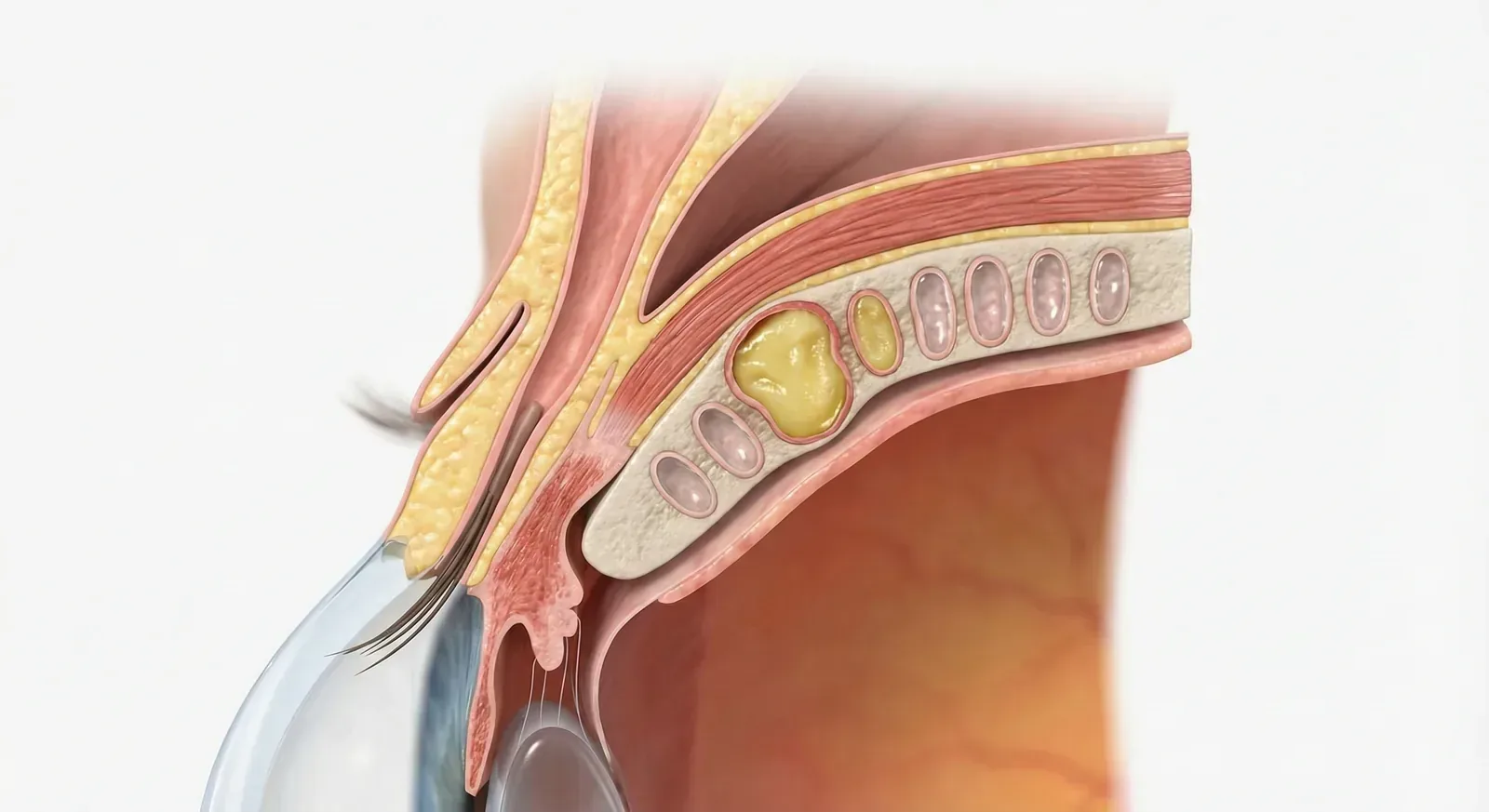
Your eyelids contain tiny oil glands (meibomian glands) that secrete an oil layer to prevent tears from evaporating. In posterior blepharitis, these glands become clogged with thickened oil, leading to dry eye symptoms and inflammation.
When to See a Doctor
While home hygiene is the mainstay of treatment, you should consult an eye care professional if:
- Symptoms do not improve after 2 weeks of daily warm compresses and hygiene.
- You experience pain, significant vision changes, or intense light sensitivity.
- The eyelids become very swollen or hot to the touch (signs of infection like preseptal cellulitis).
- You notice eyelashes falling out (madarosis).
Note: An optometrist can diagnose the specific type of blepharitis you have using a slit-lamp examination and may recommend prescription treatments if over-the-counter hygiene is insufficient.
Explore next
Related content
Continue with related guides that build on this topic and keep your care plan consistent.
